General Information
Helping Your Temporomandibular Joint (TMJ) Heal
The temporomandibular joint (TMJ) is a ball-and-socket joint located where the upper and lower jaws meet. When the TMJ and related muscles are injured, they need time to heal. Self-care is very important. You can take steps to reduce pressure on the TMJ and speed healing.
Eating with Care
Chewing strains the TMJ. When symptoms are bad, you may not be able to chew at all. To get you through times when your symptoms are worst, try these tips:
Choose soft foodssuch as scrambled eggs, oatmeal, yogurt, quiche, tofu, soup, smoothies, pasta, fish, mashed potatoes, milkshakes, bananas, applesauce, gelatin, or ice cream.
Avoid biting into hard foodssuch as whole apples, carrots, and corn on the cob. Instead, cut foods into bite-sized pieces.
Grind or finely chopmeats and other tough foods. Try hamburger meat instead of steak.
Using Ice and Heat
Your healthcare provider may suggest using ice and heat. Ice helps reduce swelling and pain. Heat helps relax muscles, increasing blood flow.
Use a gel pack or ice wrapped in a towelfor severe pain. Apply for10-20 minutes or until the site becomes numb. Repeat as needed.
Use moist heatfor mild to moderate muscle pain. Apply a moist,warm towel to the muscles for10-20 minutes. Repeat as needed.
Avoiding Triggers
Certain activities (called triggers) strain the TMJ, making symptoms worse. The tips below can help you avoid common triggers and limit strain.
Avoid hard or chewy foods,such as nuts, pretzels, popcorn, chips, gum, caramel, gummy candies, carrots, whole apples, hard breads, and even ice.
Reschedule routine dental visits,such as cleanings, if your jaw aches. If you have severe pain, call your healthcare provider.
Support your jawwhen yawning. When you feel a yawn coming on, put a fist under your jaw. Apply gentle pressure. This helps prevent wide, painful yawns.
Avoid any activity that hurts,such as nail biting, yelling, and singing.
Maintaining Good Posture
Work at improving your posture during the day and when you sleep. Good posture can help your body heal. Try these tips:
Use a headsetwhen on the telephone. Don't cradle the phone with your shoulder.
Keep ergonomics in mind.This includes making sure your workstation fits your body. Support your lower back. Take frequent breaks to stretch and rest. If you use a computer, keep the monitor at eye level.
Keep your head in a neutral position,with your ears in line with your shoulders. Don't slouch or crane your head forward.
Use an orthopaedic pillowto support your head and neck during sleep.
Date Last Reviewed:
Date Last Modified:
Pain Relief Methods for Temporomandibular Disorders (TMD)
You have been diagnosed with temporomandibular disorder (TMD). This term describes a group of problems related to the temporomandibular joint (TMJ) and nearby muscles. The TMJ is located where the upper and lower jaws meet. TMD can cause painful and frustrating symptoms. But your doctor can recommend various pain relief methods as part of your treatment. These may include medications and certain types of therapy such as massage or gentle exercise.
Using Medications

Anti-inflammatories and analgesics, which treat pain, inflammation, osteoarthritis, and rheumatoid arthritis. Anti-inflammatories reduce swelling, heat, redness, and pain. They also help restore function. Analgesics reduce pain. Nonsteroidal anti-inflammatories (NSAIDs) relieve inflammation as well as pain.
Muscle relaxants, which treat myofascial pain. This is pain that occurs in the soft tissues or muscles around the TMJ. Muscle relaxants help ease muscle tension. This reduces pressure on the TMJ from tight jaw muscles.
Antidepressants,which can be used to reduce pain or bruxism (teeth grinding). At higher dosages, these medications are used to treat depression. Given at low dosages, antidepressants help relieve TMD symptoms. They can reduce muscle pain. They also raise the level of serotonin, a body chemical that improves sleep. This in turn can decrease bruxism during the night.
Treating Painful Muscles
A trigger point is a painful spot in a tight muscle. It is often painful to the touch and may refer pain to other places. Your healthcare provider can focus on trigger points using:
Massage,both inside and outside the mouth. This relaxes muscles and improves circulation.
Palpation,which is applying pressure to points of the jaw and face with the fingers.
Cold sprayand stretching of the muscles to relax them.
An anestheticfor pain relief. This may be given as an injection by your dentist.
Treating the Joint
Therapy may focus directly on the TMJ. There are different ways to treat the joint:
A self-care programhelps you treat and manage symptoms on your own. Your program may include exercises. It may also include using ice and heat to relieve pain.
Gentle manipulationreduces pain and restores range of motion. The healthcare provider uses his or her hands to relax muscles and ligaments around the joint.
Exercisesstrengthen muscles in the jaw and face.
Ultrasounduses sound waves to reduce pain and swelling. It also improves pain and swelling.
Treating Inflammation
When the joint is inflamed, movement becomes difficult-even impossible at times. Your healthcare provider can help. Treatment may include:
Rest and gentle exerciseto increase range of motion. One common exercise is to apply pressure to the jaw and resist the movement.
A gel pack or ice wrapped in a towelapplied for10-20 minutes. This eases swelling and reduces pain.
Massage and gentle manipulationas described above.
Date Last Reviewed:
Date Last Modified:
When You Have Temporomandibular Disorder (TMD)
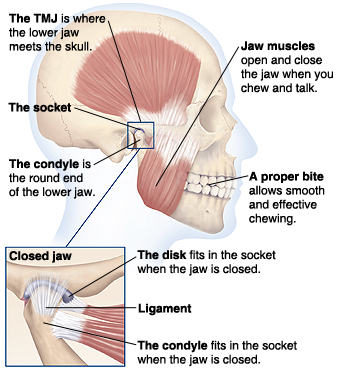
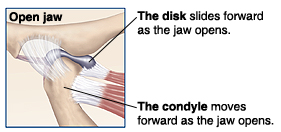
The temporomandibular joint (TMJ)is a ball-and-socket joint located where the upper and lower jaws meet. The TMJ and its nearby muscles make up a complex, loosely connected system. Because of this, a problem in one part of the system can affect the other parts. This can cause you to have temporomandibular disorder (TMD).
How the Temporomandibular Joint Works
You have one joint on each side of your mouth that together make up the TMJ. These joints are part of a large group of muscles, ligaments, and bones that work together as a system. When the system is healthy, you can talk, chew, and even yawn in comfort. Muscles contract and relax to open and close the joint. The disk absorbs pressure in the joint. It also allows the jaws to open and close smoothly. Ligaments connect the jaw bones to the skull. They also support the joint.
Common Temporomandibular Problems
When there is a problem with the TMJ and its related system, you can develop TMD. Common TMD problems include tight muscles, inflamed joints, and damaged joints.
In some cases, symptoms may be related to the teeth or bite.
Tight muscles:The muscles surrounding the TMJ can go into spasm (tighten) and cause pain. Referred pain occurs in a part of the body separate from the source of the problem. For example, pain in the face or teeth could be coming from a problem in the TMJ. Myofascial pain occurs in soft tissues, such as muscle. Trigger points in these pain areas often cause referred pain. You may feel jaw, neck, or shoulder pain.
Inflamed joints: Inflammationmay include pain, redness, heat, swelling, or loss of function. Synovitis occurs when certain tissues surrounding the TMJ become inflamed. It causes pain that increases with jaw movement. Inflamed ligaments can be caused by strain or injury. When this happens, the ligaments are unable to support the joint. Rheumatoid arthritis is a joint disease. It leads to inflammation in the TMJ.
Damaged joints:Many people hear clicking when their jaw moves. If you feel pain along with the noise, the joint may be damaged. Impingement occurs when the disk slips out of place (displacement). This causes the jaw to catch. As the disk slips, you may hear a clicking sound. Locked jaw occurs when the disk gets stuck in one position. As a result, the jaw locks open or closed. Osteoarthritis is a joint disease. It causes the TMJ to wear away (degenerate). This leads to pain during movement.
Other Problems
The parts of the jaw and mouth make up a single unit. That's whya problem in one area can cause symptoms elsewhere. Teeth or bite problems associated with TMD include:
Bruxism(grinding your teeth side to side)
Clenching(biting down on your teeth)
Malocclusion(when the teeth or bite is out of alignment)
Your healthcare provider will give you more information about these problems if needed.
Date Last Reviewed:
Date Last Modified:
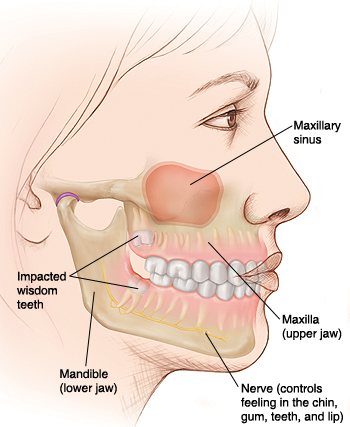
Understanding Wisdom Teeth
Wisdom teeth are very much like your other permanent teeth.The main difference is that they are the last to develop and grow in (when you're "older and wiser"). Most people have four wisdom teeth, one in each corner of the mouth. Some people naturally lack one or more of their wisdom teeth.
Wisdom Teeth and Your Dental Anatomy
There are several types of teeth. Each type is designed either for bitingor for chewing. The wisdom teeth are molars, or chewing teeth. Both the upper and lower jaws have three molars on each side. The wisdom teeth are the last in line, which is why they're called "third molars." Because there are eight other molars to do the chewing, most people can get along fine without wisdom teeth.
Anatomy of a Tooth
The crown is the part of the tooth that has a hard chewing surface. Below the gumline, the root anchors the tooth to the bone. Nerves and blood vessels enter and exit the tooth through the roots.
How Wisdom Teeth Develop
All teeth form within the jawbones. As the roots grow, thetooth's crown gradually pushes toward the gum until it erupts (breaks through the gum). After a tooth has erupted, the roots continue to lengthen. It takes years for the roots to develop completely. The jawbones become denser and more rigid over time.
Around age 9, wisdomteeth start to form inside the jawbones. The jawbones have a lot more growing to do, so they are not yet at their full density.
By the late teens, wisdom teeth roots have developed and arelengthening. The crown of each wisdom tooth may begin to erupt.
By the early 20s, each wisdom tooth haserupted or is impacted (unable to fully erupt). The roots may still be forming. The jawbones have finished growing.
By about age 40, the roots of the wisdom teeth are solidly anchored in thebone. The jawbones have reached their adult density.
Date Last Reviewed:
Date Last Modified:
Orthognathic Surgery: Recovering at Home
You just had orthognathic surgery.This istreatment that reshapes the jaws to improve their form and function. Your job now is to keep yourself comfortable and help your body heal quickly. Make sure to get plenty of calories and protein. Get up and move around, but avoid strenuous activity. Be sure to get lots of rest. Keep your mouth and teeth cleanto help the incisions heal.
Controlling Swelling and Pain
For the first few days, swelling will likely increase. It should then start to ease. To reduce swelling and pain:
Sit or lie with your head and shoulders higher than your heart.
Apply an ice pack to your face for10minutes at a time, with breaks of at least5 minutes in between. Keep a thin cloth between the cold source and your skin.
Use pain medications as directed.
Nutrition and Fluids
You will need to get enough nutrition, which may be harder while you're not able to chew. You also need fluids to help prevent dehydration and nausea. For calories, protein, and fluids, try total-nutrition drinks, protein powders, soups, milk shakes, and other blended foods. Don't use a straw, since the suction can stress the incisions in your mouth. Instead, use a glass or a "sippy cup" designed for young children. Once you can chew again, eat soft foods that can be cut with a spoon or fork.As you heal,you'll gradually return to your normal eating habits.
Keeping Your Mouth and Teeth Clean
To keep your teeth as clean as possible:
If you can't open your jaws, brush the front surfaces of your teeth with a baby toothbrush.
If a fluoride toothpaste or mouth rinse is prescribed, use it as directed.
If your surgeon advises it, start using an oral irrigator about10 days after surgery.
Aim to get back to brushing and flossing normally as soon as you can.
When to Call Your Surgeon
If you have any of the following problems, call your surgeon:
Severe bleeding
Pain that can't be controlled
Nausea or vomiting that can't be controlled
Swelling that continues to worsen after3-4 days
A fever of100.4F or higher
Go to the emergency department if your doctor's office is closed.
Date Last Reviewed:
Date Last Modified: